Vasectomy: What It Really Means, How It Works and What to Expect
03 November 2025
Deciding on male sterilisation can feel like a big step. Yet for many, a vasectomy offers a sense of clarity and relief: a once-and-for-all solution to family planning that lets you focus on life without constant worry about contraception. In this article, we explore what vasectomy truly involves, why it remains one of the most reliable forms of male contraception, how modern clinics deliver the procedure, and what to expect before, during and after the decision. This is a practical, straightforward guide written for anyone considering vasectomy and wanting to make an informed decision.
What is vasectomy and how does it work
Vasectomy is a simple surgical procedure that permanently prevents a man from fathering children by blocking the sperm from mixing with the semen that is ejaculated during sex. The procedure involves cutting or sealing the tubes — called the vas deferens — that carry sperm from the testicles to the urethra. After a successful vasectomy, the testes still produce sperm and hormones as before, but the sperm cannot exit the body: the fluid released during ejaculation no longer contains sperm. In effect this provides highly effective contraception.
Because a vasectomy does not remove any organs and does not interfere with testosterone production, sexual performance, erection, ejaculation volume, or hormone levels remain unchanged. That means a person’s sex life and bodily functions continue as before — the only difference being sperm are no longer present in the semen.
There are two common approaches to vasectomy. The traditional or conventional vasectomy uses small incisions in the scrotum to access the vas deferens. The more modern “no-scalpel vasectomy” (also known as NSV or keyhole vasectomy) uses a tiny puncture rather than a scalpel, reducing bleeding, pain, bruising, and promoting quicker recovery. Both methods are equally effective when carried out by experienced clinicians.
The decision to undergo vasectomy should always follow informed counselling. It is considered a permanent form of contraception, and while reversals exist, they are complex, expensive and do not guarantee a return to pre-vasectomy fertility. For individuals or couples confident that they do not want more (or any) children in the future, vasectomy can be a responsible, long-term choice.
Why vasectomy remains a trusted choice for family planning
Choosing a method of birth control is deeply personal. For many couples, vasectomy offers a unique blend of simplicity, reliability and minimal impact.
First, the effectiveness of vasectomy is extremely high. Once the procedure has been completed and sterility is confirmed, the chances of pregnancy are negligible. This makes vasectomy one of the most effective forms of contraception available.
Second, vasectomy avoids many of the side effects sometimes associated with female sterilisation or long-term hormonal contraception. There is no systemic hormonal manipulation, no lasting effect on libido or sexual performance, and no risk of pregnancy for the partner. For men, this can mean taking shared responsibility for family planning in a simple, one-time procedure rather than repeated or ongoing contraceptive methods.
Third, vasectomy is quick and minimally invasive. Under local anaesthetic and often using the no-scalpel technique, the procedure typically takes about 15–30 minutes. Many men are able to return home the same day and resume light daily activities within a couple of days. Full recovery is often reported within a week to ten days, with few needing more than a few days off work.
Fourth, when conducted in a reputable clinic by trained professionals, vasectomy carries a low risk of serious complications or long-term health consequences. The testes continue to produce sperm and hormones; sperm are instead naturally broken down and absorbed by the body. There is no increase in risk of cancer, heart disease or other systemic illnesses caused by vasectomy.
Finally, vasectomy can represent a thoughtful, shared decision in a relationship: it places on men a lasting opportunity to manage fertility, allowing couples to make family planning choices together in a balanced way.
What to expect before, during and after the procedure
Undergoing vasectomy involves a few important steps before, during and after the procedure. Awareness of these ensures you can approach the decision with practical clarity and realistic expectations.
Before the procedure, a thorough consultation is essential. A qualified clinician will explain what vasectomy does — and does not do. It will be made clear that vasectomy is intended as permanent contraception. Good counselling helps ensure that the decision is informed and consensual. The clinician will also assess whether you are a suitable candidate, taking into account medical history and any risk factors.
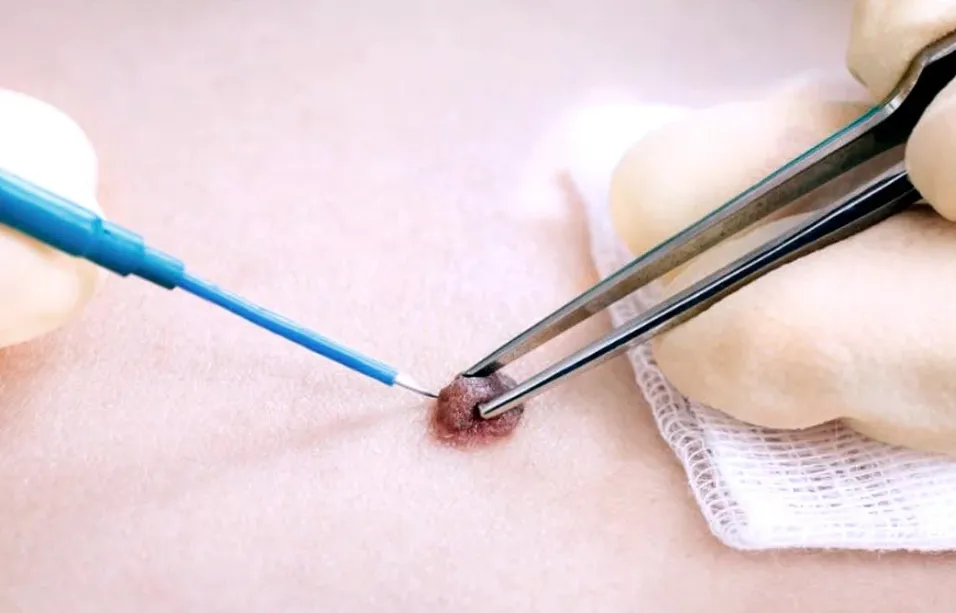
On the day of the procedure you will likely receive local anaesthetic. With the no-scalpel method, the clinician gently punctures the skin to reach the vas deferens, minimising tissue damage and allowing for faster healing. The vas deferens on both sides are then cut and sealed — via tying, cauterising or blocking — before the puncture site is dressed. The procedure is brief, often completed in half an hour or less.
After vasectomy, there is usually a short recovery period. You may experience some mild swelling or bruising in the scrotal area. There might be slight discomfort or a feeling of fullness as tissues heal. It is generally recommended to avoid vigorous physical activity or heavy lifting for at least a week. Supportive underwear and rest help with comfort during recovery.
Importantly, sperm may remain in the vas deferens for some time after the procedure. That means you must continue using alternate contraception until follow-up testing confirms there is no sperm in your ejaculate. A semen analysis, usually scheduled two to three months after the procedure, helps ensure sterility has been achieved. Only after a doctor confirms sperm count is zero should you rely solely on vasectomy for birth control.
While most recover without complications, you should also watch for signs that need medical attention — such as persistent pain, swelling, lumps, discharge, fever or signs of infection. In rare cases, small lumps called sperm granulomas may appear at the site where the vas deferens was severed. These lumps are usually harmless and may resolve over time, though they can occasionally cause discomfort. Post-operative chronic pain, known as post-vasectomy pain syndrome, is uncommon but possible.
Addressing common concerns and misconceptions
It is not uncommon for myths, fears and misconceptions to discourage men from considering vasectomy. Clarifying these concerns with accurate, evidence-based information can help individuals and couples feel more confident about their decisions.
One frequent worry is that vasectomy might affect sexual performance or hormone levels. Medical evidence shows this is not the case. The testes continue to produce testosterone and other hormones as before. Erection, ejaculation, orgasm and libido remain unaffected. The only change is that semen no longer contains sperm.
Another concern is long-term health risk. Large bodies of research have not found a clear link between vasectomy and serious conditions such as cancer or cardiovascular disease. Reviews by leading medical institutions conclude that vasectomy is safe with minimal long-term risk when performed correctly.
Some men worry about pain or recovery time. In reality, most report only mild discomfort, swelling or bruising. Recovery is typically quick, with normal daily activity possible within a few days and full recovery within a couple of weeks.
There may also be cultural or social hesitations. In many parts of the world vasectomy remains far less common than female sterilisation. In certain regions the use of vasectomy as a family planning tool has declined over decades, due to social stigma, lack of awareness or limited access to quality male sterilisation services. That can make it harder for couples to learn about vasectomy or feel comfortable choosing it.
Yet for those who understand what vasectomy really is — a safe, effective, long-term contraception method — these concerns may seem less daunting. Access to accurate information, ethical counselling and respectful, professional care can make the decision much clearer.
The value of a trusted clinic and informed care
When vasectomy is provided in a professional, medically governed clinic environment, with properly trained staff and appropriate pre-operative evaluation, the safety and effectiveness of the procedure are maximised. Clinics that follow standard protocols — including local anaesthesia, sterile surgical practices, appropriate counselling, and follow-up semen analysis — are likely to give the best outcomes.
A reputable clinic should ensure that you are given clear, honest information about benefits and risks, that consent is truly informed, and that aftercare guidance is realistic and supportive. It should prioritise patient comfort, privacy and dignity. In a world where family planning decisions are deeply personal, such an approach makes a big difference.
Vasectomy may be a permanent step, but with that comes long-term peace of mind. For many individuals and couples who are certain about their family plans, that clarity can bring relief.
Is vasectomy right for you and your partner
Deciding on vasectomy is not something to take lightly. It requires honest, open communication between partners and a clear understanding of what the procedure can — and cannot — offer.
Let yourself ask important questions: Are you confident you do not want more children? Do you understand that reversal is difficult and may not restore fertility? Are you prepared for recovery and follow-up testing? Are you comfortable with the permanent nature of sterilisation?
If the answer to these questions is yes, vasectomy can offer a highly effective, low-maintenance, long-lasting solution. It may also reflect shared responsibility between partners, giving men an active role in family planning decisions.
In the broader context, when more men consider vasectomy, it can help balance family planning responsibilities, reduce reliance on female sterilisation and relieve many of the burdens traditionally shouldered by women. It can foster a more equitable approach to contraception and reproductive health.
Conclusion
Vasectomy stands out as a simple but powerful option for permanent male contraception. It works by safely blocking sperm transport without affecting sexual function or hormone levels. When performed by trained professionals in a trusted clinical environment, vasectomy is highly effective, low risk and offers rapid recovery.
While the decision is deeply personal and permanent, the benefits may bring clarity, convenience and shared responsibility. With honest counselling, proper care and realistic expectations, vasectomy can be an informed, responsible and liberating choice for individuals or couples who have completed their family planning.
If you are considering vasectomy explore your options, understand the process, weigh the pros and cons together with your partner and medical advisor, and choose what feels right for your future.